
Bob Atkins, CEO and Founder of Gray Associates, Kay Lenhart, MSN, CNE, RN-BC (Informatics), Sarah Gabua, DNP, RN, and Kate Eby, MN, APRN, FNP, CNE, Healthcare Partners at Gray Associates.
In April 2013, the new NCLEX-RN® (the standard test required for RN licensure) was launched – and pass rates tumbled by 12 points.
DOWNLOAD ARTICLE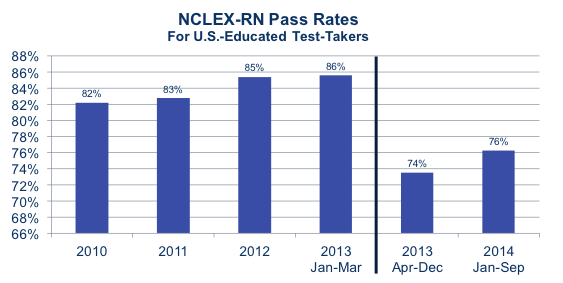
The new exam toughens grading and emphasizes concepts rather than memorization. To improve pass rates, many nursing schools are adapting their curriculum, teaching methods, and faculty to enable students to succeed on the new exam and grading curves. For those who have not made the changes, this problem is becoming increasingly urgent, as low pass rates threaten their accreditation and Board of Nursing approval. Fortunately, the problem can be fixed.
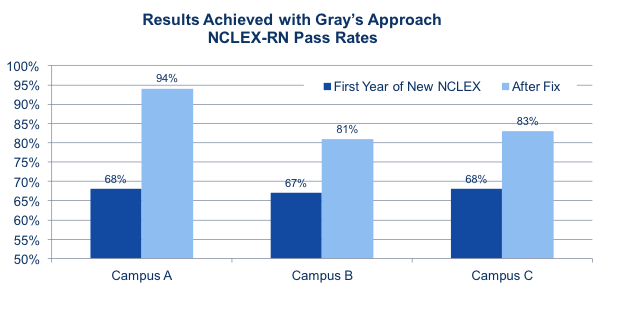
The chart on the right shows how adapting a nursing program to the new, conceptual approach can more than overcome the effects of the NCLEX-RN changes. In each of these cases, implementing the approach described in this white paper led to a 14- to 26-point improvement in NCLEX scores the next year, with all three campuses achieving pass rates over 80 percent.
Why did the NCLEX-RN change?
Traditionally, nursing programs were disease-centered. The NCSBN decided this approach had to change. Why?
In the traditional approach, students were expected to know the symptoms, risk factors, and treatments for a large number of diseases. However, with advances in medical knowledge, there are simply too many diseases and conditions to teach them all. As a result, even the best-educated nursing students faced NCLEX questions about a disease they had never been taught.
In addition, the disease-centered approach emphasized memorization, which was effective when knowledge was advancing fairly slowly and memorized facts would remain “true” for most of a career. However, science is now advancing so quickly that memorized material is quickly outdated. As a result, education now places higher value on conceptual understanding and critical thinking rather than memorization.
The role of nurses is also evolving in a way that favors critical thinking. A few decades ago, hospitals treated a high volume of minimally-acute illnesses and injuries, so it was important for nurses to be able to quickly assess and treat these conditions. In today’s world, there is a growing number of patients with two or three chronic conditions (e.g., depression and diabetes) for which they may take a variety of medications (e.g., Zoloft and insulin). To reduce costs, the routine work for these patients is now performed by less expensive care providers, such as Medical Assistants. This positions nurses to work “at the top of their licenses,” providing advanced care for patients with complex and highly individualized medical situations. In this environment, nurses must be able to make nursing diagnoses and treat specific pathologies—somewhat independently of the underlying diseases and medical diagnoses.
Technology and coordination of care are also increasing the needs for critical thinking and communication skills.
It is not enough for nurses to understand current medical technology; they must also be able to learn about the new medical technologies that will be introduced during their careers.
They also need to be able to coordinate care within and outside healthcare systems, as well as within and outside the nursing profession.
As a result of these and many other changes in healthcare, NCSBN determined that nursing instruction and testing had to evolve.
How did the NCLEX-RN change?
The new NCLEX-RN raises the minimum passing grade and requires that students understand much more about how the body works, with less emphasis on specific diseases. In essence, students must understand symptoms and pathophysiology. Once they identify the symptomology, they can use their knowledge base to select the appropriate treatment, regardless of the disease name.
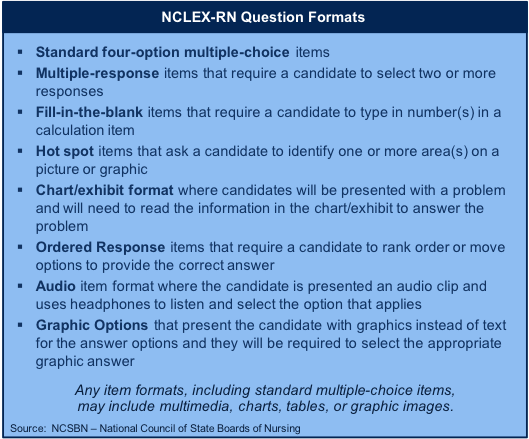
The format of the test itself has also become more sophisticated. In addition to traditional multiple-choice questions, the test now includes “multiple-response items,” where several answers may be correct. In other sections, the student may have to order or prioritize answers, highlight areas on a diagram, fill in a blank, or select among graphical options. How does nursing education need to change?
Enabling students to succeed on the new NCLEX-RN will require changes in curriculum, instruction, clinical training and simulations.
1. Curriculum
The most obvious consequence of the NCLEX change is the need to align nursing curricula with the new expectations. For example, instead of teaching each respiratory disease, the curriculum should focus on helping students understand concepts related to the respiratory system, such as gas exchange or acid/base balance. Then, once that understanding is in place, the students can understand symptoms, risk factors, diagnostics, and treatments. Because the students understand these concepts at the physiologic level, they understand the nursing process at a deeper level than they could have from memorizing disease-specific lists.
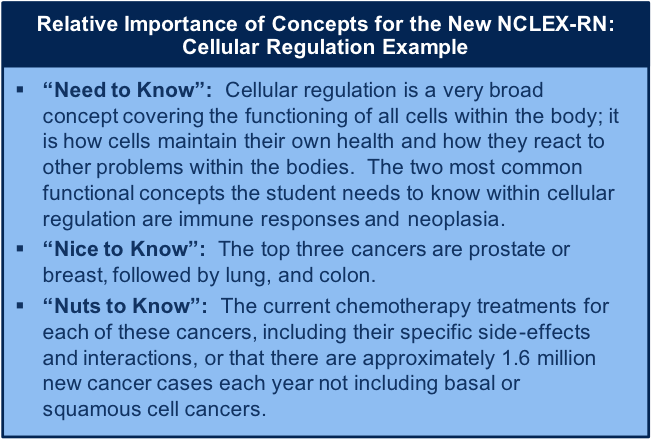
The NCLEX-RN has also changed the relative importance of the concepts that are taught. As a result, each institution has to re-assess what information is “need to know,” “nice to know,” or “nuts to know.”
As with any curriculum, each institution must assess how course content should be tailored to align with the strategic plan, mission, vision, goals and objectives of the institution. A program should have approximately 40 concepts in order to be effective; this allows the institution to pick and choose concepts that truly meet the needs of the institution, the school of nursing, and the specific nursing program. For example, all nursing programs should address some form of “oxygenation” as a concept. However, depending on the overriding philosophies and theories upon which the program is based, the concept might be called “oxygenation,” “gas exchange,” “ventilation,” or “ventilation/oxygenation and perfusion.” Upon delineating the concepts, the institution must define each concept and list exemplars that are important for the institution. In this example, an institution could choose “gas exchange” as the title of the concept and define it as “the process of oxygen and carbon dioxide being transported to and from cells through ventilation, transport, and perfusion processes.” Another institution might choose “ventilation” as the title of the concept and define it as “the physiologic processes that occur when oxygen and carbon dioxide gases are exchanged within the respiratory anatomy.” Both institutions are going to ultimately cover the same material so the student can pass the NCLEX, but each institution will have a curriculum that is well-suited to their current goals and objectives. Finally, exemplars are chosen based on the institution’s geographic location and disease prevalence. It does not make sense to use flail chest as an exemplar if traumas are all flown to a facility that students will not be close to or spending clinical time observing.
2. Nurse educators
This change in curriculum also puts a new burden on instructors. It is not the curriculum they were taught – or the curriculum they were teaching. Traditional nursing instruction methods may be less relevant, including in-class quizzes and lectures.
Mastering concepts may require new approaches, such as a “flipped classroom” where lectures are watched at home and “homework” is done in class.
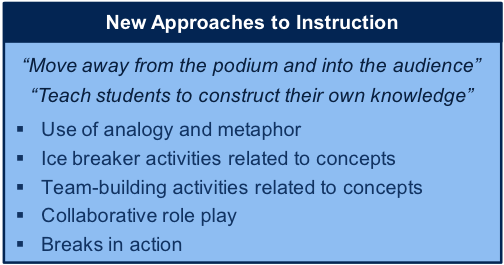
Other topics may benefit from student-directed learning or experiential learning that actively engages the student. It is not realistic to expect traditional nurse educators to suddenly switch to teaching a new curriculum using a variety of new techniques.
Replacing current nurse educators with faculty who are familiar with concept-based education is not an option. There is already a shortage of nursing faculty. Faculty retirements will make this problem worse, and the few educators who have mastered the concept-based curriculum are in high demand. As a result, schools will have to help current faculty make the transition from disease-focused education to concept-based education.
This will require coaching and educating the educators. It may require having instructors take continuing education programs to fill knowledge gaps and change attitudes about appropriate teaching strategies. It may mean a greater reliance on Certified Nurse Educators and outside experts who can help develop curriculum and coach faculty. The transition will take several years, as educators learn new skills and overcome their resistance to change—or are slowly replaced.
3. Clinicals
The new NCLEX is also driving changes in clinical instruction. Historically, clinical training enabled a variety of learning, including training on specific tasks. Now, task proficiency should be taught in labs, not in the clinical setting. Clinical learning should help nurses understand the patient in detail – transforming formal training into deeper understanding, and enabling the nurse to properly treat the patient. For example, in the past, a nurse might have sought a clinical opportunity to insert an NG tube; today, nurses should be concerned with an NG intubation only if it has been ordered for their patients. Fundamentally, clinicals are for the integration of KSAs: Knowledge (classroom learning), Skills (lab training), and a holistic Attitude to the art and science of nursing.
In many ways, arranging clinical patients for each student is easier with a concept-based curriculum. If a student is supposed to be learning about respiratory systems, the good news is that every patient has one. If a patient is hospitalized, the respiratory system – and the entire physiology of the patient – is affected by the current diagnosis, even if the diagnosis is not specifically for a respiratory disease. Critical thinking, in terms of clinical reasoning, has to occur, because students have to think about how their patient’s disease is affecting the respiratory system. The student has to take care of and understand the patient holistically and understand the underlying current symptomology. Therefore, finding the right patients for each student to work with is much less of a challenge: every patient is an appropriate patient on clinical day.
This new approach to clinical training does put different demands on the academic institution’s clinical instructor and on the healthcare facility. Clinical instructors need to ensure that students work with a variety of patients, so students can make appropriate connections to classroom and lab learning. Clinical instructors, and institutions, need to convey that students are not in the clinical site to “sign-off” on clinical tasks, but rather to process knowledge and interact with patients. If students are assigned to a floor, they should not be looked at as extra help for the day by the healthcare facility, but rather as an opportunity to guarantee that the next RNs hired will be safe, high-quality nurses. The clinical instructor will also have to learn some new techniques with assignments and pre/post-clinical activities.
4. Simulation
Shorter hospital stays and higher acuity are reducing clinical opportunities for students to learn and see the results of their actions; simulation can help fill that gap
. Simulation is also a wonderful opportunity for students to both practice skills and learn critical thinking; in effect, it is a bridge connecting the classroom, lab and clinical experiences. It should be a part of every nurse’s education and can be very effective in a concept-based curriculum. However, many schools do not use simulation appropriately.
There are different levels of simulation. High-fidelity simulation requires a school to invest, at a minimum, in a $100,000 manikin that can truly simulate a patient, including bleeding and speaking. One way to use that manikin is for the instructor to walk through a story about the manikin and demonstrate how to practice on it (e.g., take its blood pressure). However, this approach does not take advantage of the manikin’s full capabilities or its instructional value.
The proper way to use a high-fidelity manikin is to have students, in groups of two to five, practice actual healthcare provider roles as they treat the manikin. For example, one student might be the RN, another might be an LPN, another might be the nurse aide, while still another plays the Charge Nurse or Shift Supervisor. The instructor often acts as the doctor on call, and the students have to solve problems by themselves. This approach gives students the opportunity to do things they might not be permitted to do on a real patient. In this context, students can use their skills, think critically about their patients, and integrate their knowledge to treat the patient to the best of their ability. In a simulation, they can – and often do – make mistakes, from which they can learn and understand consequences, all without endangering a patient.
This simulation approach is allowed in every state to at least some degree. It protects the faculty, by reducing the risks when students practice under the faculty licenses. It also helps students use and improve their soft skills: professionalism, teamwork, and communication.
Summary
The new NCLEX-RN will cause all nursing schools to revisit and improve nursing education. Some schools have already made changes, and their students are doing well on the NCLEX-RN. Others schools still need to overhaul their programs and develop their faculty’s ability to teach a new curriculum using new methods. In all cases, there is unique and timely opportunity to take a fresh look at the nursing program and enhance the content, delivery channels, and instruction. Your life may depend on it.

Bob Atkins CEO and Founder of Gray Associates, led Gray’s entry into the education industry and the development of Gray’s proprietary industry databases and service offerings. He has worked with all of Gray’s education clients, counseling CEOs and CMOs on business strategy, pricing, location selection, and program strategy. He is an expert in business strategy, marketing, sales, and high-tech distribution channels. He has helped AT&T, Avaya, American Express, Dex Media, Qwest Communications, HP, IBM, Northcentral University, UTI, Alta Colleges, and other clients to develop growth strategies, enter new markets, and build their sales and channel organizations. He has also led efforts that have eliminated tens of millions of dollars in cost, particularly in sales and channel management. He is a published author whose articles have appeared in the Wall Street Journal, Sales and Marketing Management, and other publications around the world. He received an MBA, with honors, from Harvard Business School and a BA, magna cum laude, from Harvard College.
Contact Information: Bob Atkins // CEO and Founder // Gray Associates // 617-401-7662 // bob.atkins@grayassociates.com
Kay Lenhart MSN, CNE, RN-BC (Informatics), and Healthcare Partner at Gray Associates, is pursuing her Doctorate of Nursing Practice from Boise State University and holds a Master of Science in Nursing Education from Drexel University. She also holds a certificate in Nursing Informatics from the American Nurses Credentialing Center and is a Certified Nurse Educator through the National League for Nursing. Kay is a Certified Peer Reviewer for Quality Matters. Her clinical focus is in pediatric and informatics nursing. Her academic career is extensive: beginning with implementation of health curricula in public schools, teaching nursing in LPN, ADN, BSN, MSN, and Doctorate level coursework and programs; designing coursework and entire curricula for LPN, ADN, BSN, and MSN programs; applying, receiving, and implementing various grants; as well as developing programs for public and private, non-profit and for-profit schools and large university systems. Kay has experience in Project Management and consulting for academia, healthcare, community informatics needs, and technological design. She is a member of Phi Kappa Phi Honor Society, Sigma Theta Tau International Honor Society, Nu Eta Chapter, and was inducted as a Nurse Leader for the Sigma Theta Tau International Honor Society, Phi Pi Chapter. Other memberships and service include ANA, PSNA (current Treasurer, previous Vice-President), ANIA, NLN, AACN (invited), and AMIA. Kay has made numerous presentations at the institutional, local, regional, national, and international levels ranging in topics from technology and informatics to educational concept, curricular design, and implementation. Her DNP Scholarly Practice Project is focusing on the implementation of Evidence-Based Practice in nursing curricula and the effect of Quality and Safety, as well as improving RNs’ attitudes towards EBP and research.
Sarah Gabua, DNP, RN, and Healthcare Partner at Gray Associates, has a Doctorate of Nursing Practice from Walden University and holds various educational positions as an adjunct nursing professor in online Nursing programs. She has earned a Master of Science in Nursing in Leadership and Management, as well as a post-graduate certificate in Nursing Education from Walden University. Sarah also has experience in Nursing and Allied Health program and course development, continuing adult education, and as a CNA clinical instructor. She has a certification in distance education. Sarah has eight years of bedside nursing experience with a concentration in cardiology. She is a member of Sigma Theta Tau Phi Nu chapter, Sigma Theta Tau International Honors Society and the Golden Key International Honour Society. She currently serves as a board member of her state professional nursing organization. She was appointed to serve as the National League of Nursing Ambassador as well as the ANA Illinois Legislative Committee. Sarah has presented at various Nursing conferences on the topic of Patient/Visitor Violence towards the Healthcare Worker.
Kate Eby, MN, APRN, FNP, CNE, and Healthcare Partner at Gray Associates, has a Master’s degree in Nursing with a focus as a family nurse practitioner from Montana State University – Bozeman. Her clinical focus is in internal medicine and adult health. She has certificates in nursing education and in distance learning technologies, and is a Certified Nurse Educator through the National League for Nursing. She has held positions as a faculty member in both public and private online nursing programs. She has experience with course and program development, as well as course evaluation as a Peer Reviewer and Master Reviewer with Quality Matters. She is a member of Sigma Theta Tau International Zeta Upsilon chapter, the American Nurses Association, the Montana Nurses Association, and the American Academy of Nurse Practitioners. Kate has served on the editorial board for the Montana Nurse’s Association newsletter and the Sigma Theta Tau Zeta Upsilon Board of Directors and Scholarship Committee.










